History: An 8 year old girl presented to CSC with a chest wall and spine deformity. Her grandmother explains the deformity has been worsening she was one years old and getting worse each day. The child has no pain. The child has not had menarche.
She was born at full term, normal pregnancy and delivery and second child in the family. No other positive family history of deformity.
On examination, she had normal intellectual development, a birth mark over her trunk. The waist crease was asymmetrical. Adam’s forward bend test demonstrated obvious deformity. No other examination was documented.
Dr Saqib: Learning point 1: Scoliosis is a common case seen at CSC as it is one of the only centres in Cambodia offering surgery. It is important to understand there are different causes of scoliosis, and each cause must be considered when taking a history from your patient. In broad terms of causes, there is congenital, neuromuscular, idiopathic, traumatic, tumour, infection and degenerative.
Idiopathic is often further divided into age group (Infantile – ages 0 to 3, Juvenile – ages 4 to 10, Adolescent idiopathic scoliosis – ages 11 to 18). Adolescent idiopathic scoliosis is the most common form of scoliosis.
You can read about the different types of scoliosis here. It is important to be aware of them all when you review a patient at CSC.
Congenital
Neuromuscular
Idiopathic – infantile
Idiopathic – juvenile
Idiopathic – adolescent
Pathalogical
Adult Degenerative
Remember the prognosis of how quickly a curve will deteriorate depends on the patient’s age and growth spurt. Asking about menarche in females is important as prior to menarche there is likely to be significant growth remaining. Growth stops on average 1.5 years after onset of menarche and therefore you should ask at what age it started. Another way to assess remaining growth is the Risser classification, looking at the apophysis of the iiac crest. Risser 0 or 1 stage indicates a significant growth remaining and therefore worse prognosis for the scoliosis. Here is a link to the Risser staging on x-ray.
Dr Saqib: Learning point 2: Performing a complete examination is very important, including a full neurological examination. Here is a good youtube video on examining a paediatric spine.
And more specifically, here is the Adam’s forward bend test. This is a good screening test for scoliosis.
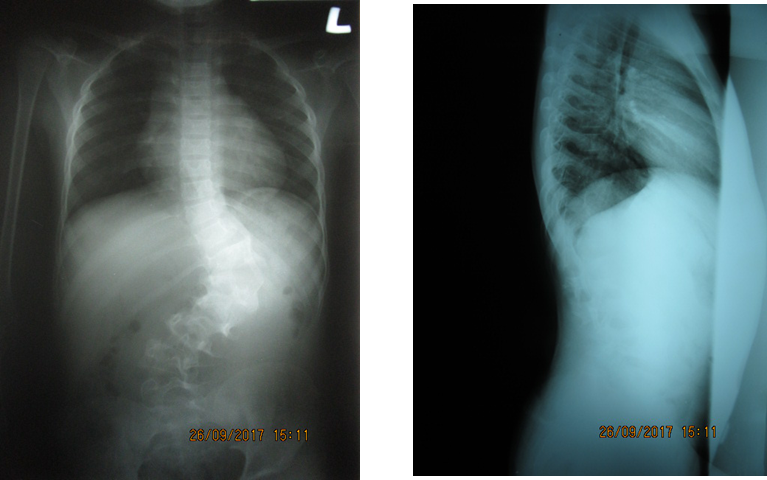
Analysing the x-ray is important in determining the severity of the curve. The angle of the curve again also helps determine the prognosis. The Cobb angle is the measurement we need to take. A description of how to measure the Cobb angle is here. You can also download a scoliometer on an app on your phone.
Once you have the complete history, examination and x-rays, then you can work out the cause of the scoliosis and plan for the best treatment. Our patient’s scoliosis began when the child was one year old – this could mean the scoliosis could be a congenital abnormalilty, a neuromuscular problem or infantile idiopathic scoliosis. We did not complete a neurological examination so this is not helpful.
The patient has a cobb angle of 65 degrees which is severe. Also there appears to be abnormalities of the vertebra in the thoracolumbar junction. Remember the different types of congenital abnormalities – failure of formation, failure of segmentation or a mixture. There appears to be some fusion between the L1-L3 verterba and a wedge shape of T12. Perhaps there is an unsegmented bar or hemivertebra that has gradually worsened and now the vertebra are becoming difficult to distinguish.
The child has a severe scoliosis that is worsening and therefore must be investigated and treated soon. In the first instance, a CT scan to evaluate the vertebra abnormalities and an MRI to assess for spinal cord tethering / syrinx would be the most important step to plan treatment.
Dr Saqib: Learning point 3: Here is a 1982 research article describing the natural history of congenital scoliosis. It is likely patients at CSC with congenital scoliosis will present late therefore reading the progression of congenital scoliosis will help us understand our patients. Look at the x-rays in the article with thoraco-lumbar congenital scoliosis – does it look similar to our patient?
[gview file=”http://teaching.csc.org/wp-content/uploads/2017/10/10.1097@00004623-198264080-00003.pdf”]